Since the dawn of human consciousness, time has remained one of the most elusive concepts. It resists comprehension not merely because it flows in silence, but because we experience it inwardly before we measure it outwardly. Humanity binds time to minutes and hours, yet lives by another kind of time: hidden, internal, a rhythm that governs hunger and sleep, attention and emotion, memory and illness. This is not astronomical time or a by-product of the Earth’s rotation, but a biological time of its own, inscribed in every cell and obeyed by every organ, from the heart to the brain.
Deep within the tissues, in a silence no ear can detect, microscopic clocks revolve. They are composed of genes that interlock in self-regulating loops, rising and falling in 24-hour cycles attuned to light and darkness, wakefulness and sleep, activity and rest. It is as though every living creature carries within itself a miniature Earth orbiting its private sun. This inner clock is not a biological luxury; it is the very condition of life. It tells cells when to labour, when to pause, when to reorganise, clear debris, or repair damage.
Even the brain, the seat of consciousness and memory, cannot function outside this temporal order. Memory does not arise at any hour, and concentration does not peak at random. Sleep is not merely a suspension of awareness, but a vast internal operation through which cells recalibrate their functions and restore balance to their synaptic connections.
Biological time, therefore, reveals itself not simply as an internal clock but as a system of identity. We are temporal beings before we are rational ones. And here lies the painful paradox: if time enables the brain to build memory and consciousness, what happens when the brain is struck by a disease that corrupts its inner time?
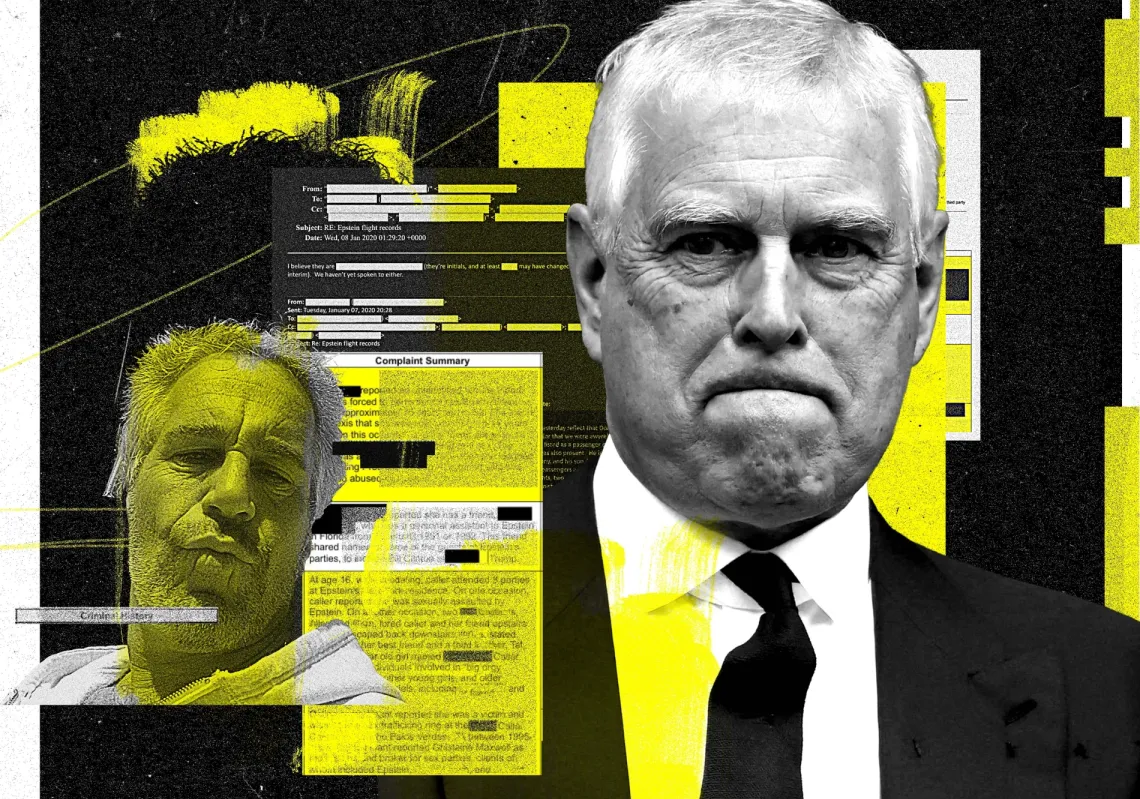
Alzheimer’s enters precisely at this point. It is not merely a disorder of memory, but a radical alteration in the architecture of time within the brain. Recent studies suggest that the earliest symptoms do not begin with the loss of recollection, as often assumed, but with the disruption of daily rhythms: disturbed sleep, nocturnal agitation, decline in evening faculties, erosion of temporal awareness. It is as though inner time fractures first, and only then do memory and identity begin to unravel.

The disrupted biological clock
Most striking of all is that the very cells charged with cleansing the brain of plaques, microglia, and astrocytes depend on a daily rhythm to carry out their work. At night, they function most efficiently, devouring protein waste and clearing amyloid deposits. But when the biological clock falters, these cells lose their timing, fall into functional paralysis, and the brain becomes a landscape where plaques accumulate unchecked.
In the face of such a disease, a scientific and philosophical question emerges with startling clarity: does Alzheimer’s truly begin when the brain ceases to remember itself, or when it ceases to know the hour?
The study of circadian rhythms within the brain reveals a powerful truth. The battle in Alzheimer’s is not only against plaques that obstruct memory, but against a collapse of time itself: the time of cells, of consciousness, of human existence. Scientific inquiry thus becomes not just a pursuit of understanding, but a quest to restore time to the brain, to recover memory, identity, and the self.
Researchers at Washington University School of Medicine in St Louis have provided direct evidence of how Alzheimer’s distorts biological time within the brain. A recent study on mice, published in Nature Neuroscience, revealed that the disease disrupts the daily rhythm inside two critical cell types responsible for clearing toxic plaques.